Biomarker Predicts Nonresponse to CAR T in Pediatric ALL
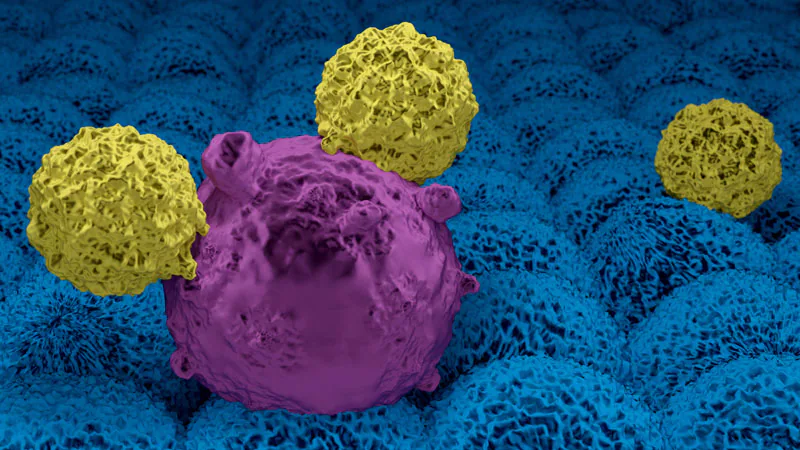
NEW ORLEANS – A new biomarker based on stem cell epigenetic signatures could help identify children and young adults with relapsed or refractory acute lymphoblastic leukemia (ALL) who would likely not benefit from chimeric antigen receptor T-cell (CAR T) therapy .
The researchers coined the term “stem cell epigenome with multilineage potential” (SCE-MLP) for the novel biomarker candidate for antigen-independent, primary non-response to CD19-targeted CAR T therapy in children with ALL.
The SCE-MLP signature is characterized by 238 differentially methylated regions, an associated stem cell-like phenotype, inherent plasticity, preservation of a B-line ALL phenotype that also harbors features of myeloid cells and stem cells, and reduced expression of involved genes in antigen presentation and processing, the team reported.
“Most importantly, this can be detected prior to therapy, so this highlights its potential use as a biomarker for response, and we hope this could improve patient selection and eligibility,” said lead author Katherine E. Masih, BS , from the Department of Genetics at the Center for Cancer Research at the National Cancer Institute (NCI).
The new findings also point to potential strategies for overcoming resistance in these patients, Masih noted. For example, pretreatment with epigenetic modulators such as hypomethylating agents could sensitize SCE-MLP ALLs to CAR T therapy.
The new findings were presented in a mini-symposium and highlighted at a media briefing here at the American Association for Cancer Research (AACR) 2022 annual meeting.
“I think it’s incredible work and incredible potential, so we need more studies in this area,” said Ana Maria Lopez, MD, MPH, professor and vice chair of medical oncology and chief of medical services at Sidney Kimmel Cancer Center- Jefferson Health New Jersey in the Municipality of Washington, New Jersey.
Lopez, who led the briefing, noted that the biomarker is valuable not only because of its ability to identify patients who are unlikely to benefit from CAR T therapy, but also because it can identify patients who will respond to CAR T therapy. therapy, for whom it is possible to de-escalate therapy.
Study details
Masih and colleagues noted that most research on resistance mechanisms to CAR T therapy has focused on relapse after an initial response. However, they were interested in the problem of primary non-response, defined as progressive CD19 positivity despite CD19 direct CAR expansion within 63 days of infusion.
“We asked the question, what characterizes patients who do not respond to CD19 CAR T cell therapy? And we hypothesized that primary non-responders to CD19 CAR T cell therapy have marked leukemia compared to patients who do respond and that these differences could be detected prior to treatment,” Masih said.
To test this hypothesis, they examined leukemia samples from 14 children and young adults with B-ALL who were undergoing treatment at Seattle Children’s and who received CD19 CAR T therapy in the PLAT-02 clinical trial. In this trial, patient responses were monitored by flow cytometry.
The samples were then stratified by response or lack of response. Samples from patients who showed no expansion of CD19 CAR T cells were excluded on the assumption that the CAR T product itself was defective.
The researchers also subjected pre-processed bone marrow samples to a variety of analyses, including genomics, transcriptomics, epigenomics, and also ATAC-seq (Assay for Transposase-Accessible Chromatin using sequencing), a technique for assessing genome-wide accessibility of chromatin and DNA methylation.
Differential methylation
The team identified gene regulatory mechanisms in which cells of responders differed from those of non-responders, including hypermethylation of genes known to be repressed in embryonic cells and cancer stem cells.
Cells resistant to CAR T had regions of open chromatin characteristic of stem cell proliferation and had patterns similar to those of hematopoietic progenitor cells and myeloid progenitor cells.
In a press release, senior author Javed Khan, MD, deputy chief of genetics at NCI, noted that previous studies have shown that a switch from lymphoid to myeloid lineage (as seen, for example, in acute myeloid leukemia [AML]) has been shown to be a resistance mechanism to CAR T therapy.
“Interestingly, we saw subpopulations of cells expressing both lymphoid and myeloid markers, indicating that the epigenomes of some unresponsive leukemias may contain a hybrid population of cells with a hybrid of ALL and AML epigenomes,” said Khan. “Our data suggest that these leukemias, characterized by both lymphoid and myeloid-specific accessible regions, are likely to be less differentiated than responsive leukemias.”
Cells that did not respond to CAR T therapy also showed reduced expression of genes encoding antigen presentation and processing pathways, indicating a reduced T cell response.
The study was funded by NIH, the Seattle Children’s Research Institute, Stand Up to Cancer, Strong Against Cancer, Alex’s Lemonade Stand, the St. Baldrick’s Foundation and the NIH Oxford-Cambridge Scholars Program. Masih, Khan and Lopez have not disclosed any relevant financial relationships.
2022 American Association for Cancer Research (AACR) Annual Meeting: Abstract 3581. Presented April 12, 2022.
Neil Osterweil, an award-winning medical journalist, is a long and regular contributor to Medscape.
For more news, follow Medscape on Facebook, Twitter, Instagram and YouTube.

Comments are closed.